Prostatic Artery Embolization (PAE) is a minimally invasive, non-surgical technique that helps improve urinary symptoms caused by an enlarged prostate or benign prostatic hyperplasia (BPH). Embolization has been performed successfully for several decades in Interventional Radiology.
The procedure is performed by an interventional radiologist rather than a surgeon, and it’s an alternative to a TURP (transurethral resection of the prostate) operation.
How It Works
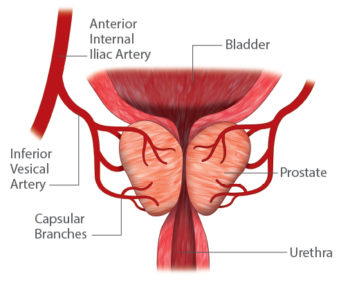
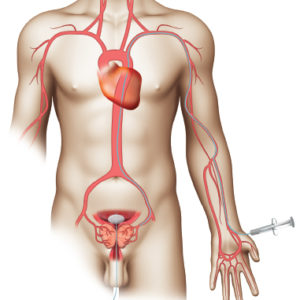
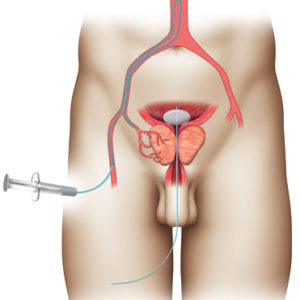
PAE is performed through a tiny hole in the groin or wrist. A catheter is inserted through the artery and directed toward the prostate. Once the catheter is positioned in the artery supplying blood to the prostate, tiny particles are then injected to plug up the artery, blocking blood flow. This is called embolization. The process is then repeated on the other side, most commonly through the same original puncture. The procedure can take anywhere from 1-3 hours, depending on the location and size of the prostatic arteries.
PAE blocks blood flow to the areas of the prostate that are most affected by benign prostatic hyperplasia (BPH), resulting in death, or necrosis, of isolated areas. Because it is impossible to block all of the blood flow to the prostate, it does not die completely. These areas of necrosis cause the prostate to initially be softer, alleviating some of the pressure that is causing blockage of the urine. Over several months, the body’s immune system reabsorbs the dead tissue and replaces it with a scar. This scar tissue slowly contracts, resulting in shrinkage of the prostate. Over six months, the prostate will shrink by 20-40%, resulting in improved and less frequent urination. Most patients see improvements of their symptoms within 30 days of the procedure.
Does It Hurt?
PAE is usually performed as an outpatient procedure, and no general anaesthesia is required. During the PAE procedure, also known as prostatic artery embolization, you’re given a mild sedative, but remain awake. Most patients experience no symptoms during the procedure, but some may experience mild pain, burning, or a hot feeling of the urethra or around the anus, which are easily controlled by the appropriate medication. In general, after the PAE procedure, the patient can get out of bed and is encouraged to urinate. Usually, patients are discharged home the same day of the procedure.
Discover the key advantages of PAE.
Key Advantages.
PAE is a safe treatment option for men with benign prostatic hyperplasia (BPH) and, like other minimally invasive procedures, has significant advantages over conventional surgery.
Some Advantages of PAE
- PAE is performed under local anaesthetic with minimal intraprocedural or postprocedural discomfort
- Minimally invasive procedure
- Can be performed as an outpatient procedure
- Relieves lower urinary tract symptoms (LUTS)
- Urethral catheterization is either not required or only for a short duration during/after the procedure
- The subsequent return to normal activities and work is rapid and immediately
- Can improve LUTS without surgery or the risk of sexual side effects or incontinence
- Overall significant improvement in the quality of life
- PAE works well for patients in whom other surgical options are not ideal or are potentially excluded.
- Carrying out PAE before considering surgery is a possible treatment strategy.
- Some center have described PAE as a planned preparatory step prior to TURP in patients with large prostates.
Understand the risks of PAE
Although PAE complications are very rare, any medical procedure carries some degree of risk. Despite the low-risk factor, it’s essential to understand the potential complications associated with PAE. These include:
- Embolization of non-target areas (i.e., bladder, rectum)
- Temporary small amounts of blood in urine and stool mixed with mucus, and blood in semen
- Potential skin burns from prolonged fluoroscopy (imaging)
- Exposure to contrast dye can cause an allergic reaction or kidney damage
- Patients with other surgical indications such as bladder calculi, diverticula or previous pelvic radiotherapy are also unsuitable for PAE
- “Post-PAE Syndrome” can last two to three days following the procedure and can include nausea, vomiting, diarrhoea, fever, pelvic pain
- Temporary painful or difficult urination
- Temporary urinary frequency
- So far, results with PAE appear variable and operator dependent, although concerted educational mentored programs are attempting to improve the reproducibility of PAE
- PAE also involves ionizing radiation whereas standard surgical therapies do not; the dose area product per procedure is around 17,400 μGy/m2, or an effective dose of approximately 47 mSv
- The technique does not enable tissue sampling, and atherosclerotic or tortuous prostatic vessels can present obstacles during PAE.